Adenoidid is a practical label used to discuss inflammation or ongoing problems of the adenoids (the pharyngeal tonsils) — essentially the same clinical space covered by the medical term adenoiditis. Because “adenoidid” appears in online searches and community conversations, this guide treats it as a modern search term aligned with classic ENT conditions. The adenoids are small lymphatic tissues in the nasopharynx that help trap germs and aid the immune system, and when they swell or become chronically inflamed, symptoms and complications can follow.
Clinically, adenoiditis is the standard diagnosis for acutely inflamed adenoids. Adenoidid functions as a user-facing keyword — helpful for SEO and patient education — but the underlying concerns (swelling, infection, obstruction) are the same. This article uses both terms interchangeably while keeping recommendations grounded in evidence-based ENT practice.
Search patterns and lay discussion sometimes invent or adapt medical words. “Adenoidid” is one such variant that can help bring attention to adenoid-related issues on health blogs and parent forums. Using it strategically in trusted, expert-backed content helps people find accurate information and feel empowered to act.
Clear knowledge about adenoid function, warning signs, and treatment options reduces anxiety, shortens time to correct care, and improves outcomes — especially for children, where airway and ear health affect sleep, learning, and development.
2. Understanding the Adenoids
Location and Function of Adenoids in the Human Body
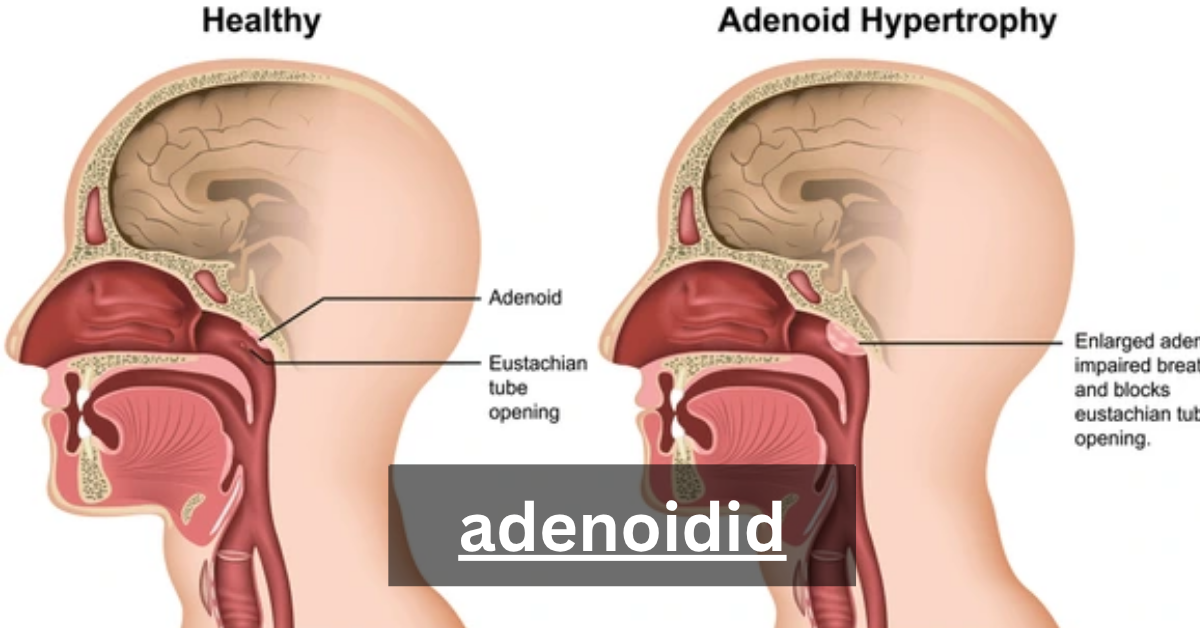
Adenoids (pharyngeal tonsils) sit high in the back of the nasal passage — the nasopharynx — near the openings of the Eustachian tubes. They are part of the lymphatic system and contribute to the body’s early immune response by trapping bacteria and viruses that enter through the nose and mouth. In childhood they are larger and more active; they tend to shrink after about age 5 and usually regress in adulthood.
The Role of Adenoids in the Immune System
As lymphatic tissue, adenoids produce immune cells and antibodies that help recognize pathogens. Their role is particularly important in early childhood when the immune system is learning to distinguish common microbes. However, frequent exposure to pathogens or repeated infections can cause persistent inflammation (adenoiditis) or hypertrophy (enlargement), which then impairs their function.
How Adenoids Protect Against Infections
Adenoids sit strategically to filter inhaled organisms; they are like a first line of defense for the upper respiratory tract. This positioning means they often encounter pathogens first — which is effective immunologically but also explains why they can become chronically infected or serve as a reservoir for recurrent infections.
Common Problems Related to Adenoid Inflammation
When adenoids swell, they can cause nasal obstruction, post-nasal drip, middle ear problems (through Eustachian tube blockage), and contribute to sleep-disordered breathing or pediatric obstructive sleep apnea. Chronic adenoid issues can lead to more doctor visits, antibiotic courses, and sometimes surgery.
3. What Exactly Is Adenoidid?
Defining Adenoidid in Simple Terms
In straightforward language, adenoidid describes swollen or infected adenoids that cause symptoms — nasal blockage, snoring, recurring ear infections, or chronic nasal congestion. Whether you call it adenoidid or adenoiditis, the practical concerns and management pathways are similar.
Cleveland Clinic
Is Adenoidid a Medical Condition or a Modern Term?
Medically, clinicians use adenoiditis and related diagnoses (adenoid hypertrophy, obstructive sleep apnea due to enlarged adenoids). Adenoidid operates primarily as a searchable, user-friendly term to capture public queries and improve access to accurate information. Think of it as a bridge between patient language and medical terminology.
The Connection Between Adenoidid and Respiratory Health
Because adenoids sit in the nasopharynx, any swelling directly affects airflow through the nose and into the lungs. This can cause mouth breathing, reduce air filtration and humidification, and worsen chronic nasal breathing problems and rhinitis. These effects ripple into sleep quality and speech patterns in children.
How Adenoidid Impacts Daily Breathing and Sleep
Enlarged adenoids narrow the airway during sleep, often causing snoring or pauses in breathing (sleep apnea). Over time, poor sleep quality can affect daytime behavior, attention, and learning in children. Addressing adenoid-related obstruction often improves sleep, mood, and daytime functioning.
4. Causes and Risk Factors of Adenoidid
Common Infections That Trigger Adenoidid
Viral upper respiratory infections and bacterial infections are the most common triggers for adenoid inflammation. Repeated infections can keep the tissue chronically inflamed. Allergies and acid reflux are also recognized contributors that can irritate adenoid tissue.
Bacterial vs. Viral Causes of Inflammation
Viral infections often precede acute swelling and may resolve on their own; bacterial infections may require antibiotic therapy (for example, amoxicillin when appropriate). Distinguishing viral from bacterial causes depends on clinical features and, occasionally, throat culture tests or specialist assessment. Always follow a clinician’s guidance before starting antibiotics.
Environmental and Genetic Influences
Environmental factors — including pollution, tobacco smoke exposure, and recurrent community infections — increase the likelihood of enlarged or chronically inflamed adenoids. Genetic predisposition to larger lymphatic tissue or allergic tendencies may also play a role. Adults with adenoid hypertrophy commonly present with histories of chronic exposure or long-standing allergic disease.
Allergies, Pollution, and Recurrent Infections
Allergic rhinitis can cause persistent nasal inflammation that keeps adenoids irritated. Pollution and secondhand smoke impair local mucous membrane defenses and increase infection risk. Reducing allergens and improving indoor air quality are practical preventive strategies.
Why Adenoidid Is More Common in Children
Children’s adenoids are proportionally larger and immunologically active, making them more likely to swell. The combination of developing immune systems and high exposure to pathogens in daycare or school settings explains the elevated incidence in young children. Adenoids usually shrink by adolescence, making adult adenoid disease less common but still possible.
5. Signs and Symptoms to Watch For
Nasal Blockage and Chronic Congestion
Persistent nasal obstruction is one of the hallmark signs of adenoid-related problems. When the nasopharynx is partially blocked, children breathe through their mouths, have nasal speech changes, and experience chronic congestion that doesn’t fully respond to typical cold treatments. Nasal saline irrigation can ease symptoms but may not resolve structural blockage.
Snoring, Mouth Breathing, and Sleep Apnea
Snoring, mouth breathing at night, and daytime sleepiness or behavioral changes suggest airway compromise. In children, obstructive sleep apnea caused by enlarged adenoids and tonsils can lead to poor school performance and hyperactivity; evaluation by an otolaryngologist or pediatrician is recommended when sleep-disordered breathing is suspected.
Persistent Sore Throat or Ear Pain
Frequent sore throats or recurrent otitis media (middle ear infections) may be related to adenoid tissue acting as a reservoir of infection or blocking the Eustachian tube, causing fluid buildup. Otitis media with effusion (fluid without active infection) is particularly linked to adenoid problems in children.
Difficulty Swallowing and Voice Changes
Large adenoids can alter voice resonance (nasal quality) and make swallowing feel awkward. While these signs alone aren’t diagnostic, in combination with snoring and nasal blockage they point strongly to adenoid hypertrophy.
Behavioral and Cognitive Signs in Children
Chronic sleep disruption from adenoid-related obstruction may produce daytime fatigue, irritability, attention difficulties, and learning problems. Parents often notice behavioral shifts that improve after targeted treatment (medical or surgical).
6. How Adenoidid Affects Children and Adults Differently
Why Children Are More Prone to Adenoidid
As noted, children have larger adenoid tissue and more exposure to pathogens in group settings. Their Eustachian tubes are shorter and more horizontal, making ear complications more likely when adenoids are enlarged. This combination raises the rate of symptomatic adenoid disease in childhood.
Impact on Speech, Growth, and Immunity in Kids
Severe, untreated adenoid obstruction can alter speech resonance, interfere with restful sleep (affecting growth hormone secretion), and occasionally correlate with weight and developmental issues due to chronic poor sleep or recurrent infections. Addressing the problem early often yields measurable improvements.
Adult Adenoidid: A Rare but Real Concern
Adults can have adenoid hypertrophy due to chronic infection, allergies, smoking, or pollution. Although rarer because adenoids typically regress, adult cases can cause persistent nasal obstruction, post-nasal drip, and chronic rhinosinusitis that requires ENT evaluation. Studies show environmental and chronic inflammatory contributors are common in adult presentations.
Misdiagnosis: Adenoidid vs. Sinusitis in Adults
Because symptoms overlap, adult adenoid disease is often misdiagnosed as chronic sinusitis or allergic rhinitis. ENT examination, nasal endoscopy, and imaging help differentiate conditions and guide appropriate management.
7. Diagnosis and Medical Examination
How ENT Specialists Identify Adenoidid
An otolaryngologist (ENT specialist) performs a focused history and physical exam, asking about snoring, recurrent ear infections, sleep problems, and nasal obstruction. Pediatricians and family physicians often refer to ENT when symptoms are recurrent or when ear and sleep complications appear.
Physical Examination and Nasal Endoscopy
Nasal endoscopy — a quick office procedure — allows direct visualization of the nasopharynx and adenoid size. For children this may be done with a flexible scope; it helps distinguish adenoid hypertrophy from other causes and assesses obstruction severity. Endoscopy can also reveal signs of chronic inflammation or pus-filled tissue.
Imaging Techniques (X-rays, CT Scans)
X-rays of the lateral neck are sometimes used to estimate adenoid size, while CT scans are reserved for complex cases or when other nasal pathology is suspected. Imaging complements endoscopy but is not always required for straightforward clinical decisions.
Laboratory Tests and Bacterial Cultures
If recurrent bacterial infection is suspected, throat culture tests or swabs from the nasopharynx can guide antibiotic selection. Routine blood tests are not typically necessary unless systemic illness is present. Culture-directed therapy helps reduce unnecessary antibiotic use.
Differential Diagnosis: Tonsillitis, Sinusitis, and More
ENT teams distinguish adenoid problems from tonsillitis, chronic sinusitis, allergic rhinitis, and foreign body issues. Tonsils are lower in the throat; adenoids are higher in the nasopharynx. Many cases involve combined adenoid and tonsil enlargement (adenotonsillar hypertrophy), which alters the treatment plan.
8. Medical Treatments for Adenoidid
When Antibiotics Are Necessary
Antibiotic therapy (commonly amoxicillin or other agents based on local resistance patterns) is used for bacterial adenoiditis or secondary infections. Many mild viral flares resolve without antibiotics, so clinicians weigh clinical signs and, if available, culture results before prescribing. Avoid self-prescribing antibiotics.
Nasal Corticosteroids and Decongestants
Topical nasal corticosteroids reduce inflammation and may shrink adenoid tissue modestly over time, improving nasal breathing. Decongestants provide short-term relief but are not ideal for long-term management, especially in young children. Nasal saline irrigation is a safe adjunct to clear mucus and soothe mucous membranes.
Pain Relievers and Anti-Inflammatory Medications
Pain relievers such as paracetamol (acetaminophen) or ibuprofen help manage throat pain and fever during acute episodes. These medications treat symptoms but do not eliminate underlying infections when bacterial causes require antibiotics.
Managing Recurrent Adenoid Infections
For repeated infections, clinicians explore contributing factors (allergies, immune issues, exposure to smoke) and may recommend targeted therapies, environmental changes, or ENT referral for consideration of surgical options. Preventive strategies are prioritized to reduce antibiotic courses and recurrent illness.
The Role of Probiotics and Immune-Boosting Supplements
Some evidence suggests probiotics and good nutrition support mucosal immunity, but supplements are adjuncts rather than primary treatments. Discuss any supplement with a pediatrician or immunologist, especially for young children.
9. Surgical Intervention: Adenoidectomy Explained
When Surgery Becomes the Best Option
Adenoidectomy (removal of adenoids) is typically recommended when medical therapy fails, when there are recurrent ear infections or persistent otitis media with effusion, or when adenoids cause significant obstructive sleep apnea. Combined adenotonsillectomy is common when both tonsils and adenoids contribute to obstruction. Evidence supports surgery for selected children with recurrent otitis media or sleep-disordered breathing.
The Adenoidectomy Procedure Step-by-Step
Adenoidectomy is usually a short (about 20–30 minute) procedure performed under general anesthesia. The surgeon removes adenoid tissue through the mouth — no external incisions — and most patients go home the same day. Modern techniques minimize bleeding and recovery time.
Recovery Time and Post-Surgical Care
Recovery is typically quick: throat pain for a few days, temporary nasal stuffiness or bad breath, and gradual return to normal activity within about a week. Some protocols recommend two weeks off school or daycare for full healing and to reduce infection risk. Pain control, hydration, and avoiding strenuous activity help a smooth recovery.
Risks, Benefits, and Long-Term Outcomes
Adenoidectomy is generally safe with low complication rates. Benefits include improved breathing, fewer ear infections, and better sleep. Risks — rare but real — include bleeding, infection, and temporary voice changes. The decision to operate balances symptoms, quality of life, and alternative therapies.
Myths About Adenoid Removal
A common myth is that removing adenoids “weakens” immunity long-term. In reality, the immune system has many redundant components, and evidence shows removal improves health outcomes when indicated without causing lasting immune deficiency. Discuss concerns with your pediatrician or ENT for personalized reassurance.
10. Home Remedies and Natural Relief
Steam Inhalation and Warm Compress Techniques
Steam inhalation may relieve nasal congestion and loosen mucus, providing symptomatic relief during flares. Warm compresses can soothe throat discomfort. These supportive measures help comfort but are not substitutes for medical evaluation when infections are suspected.
Saltwater Gargles and Nasal Saline Sprays
Gentle saltwater gargles reduce throat irritation, while nasal saline irrigation helps clear mucus and soothes the mucous membrane. These are safe, low-cost measures that support recovery and comfort in both children (with supervision) and adults.
Hydration and Immune-Strengthening Foods
Staying well-hydrated, eating nutrient-rich foods (lean protein, fruits, vegetables), and maintaining vitamins through diet support the immune system. While no single food prevents adenoid disease, overall nutrition matters for resilience against infections.
Herbal Support: Turmeric, Ginger, and Honey
Some families use turmeric, ginger, and honey for their mild anti-inflammatory and soothing properties. These can be adjunctive comforts — for example, honey for throat soreness in children older than 1 year — but they should not replace doctor-recommended therapies for bacterial infections or severe obstruction.
Avoiding Environmental Irritants and Allergens
Reducing exposure to tobacco smoke, indoor pollutants, and known allergens decreases chronic irritation. Using air purifiers, managing pets, and controlling indoor humidity can make a meaningful difference in symptom frequency and severity.
11. Preventing Recurrence of Adenoidid
Maintaining Nasal Hygiene and Air Quality
Regular nasal saline rinses, prudent hand hygiene, and reducing exposure to secondhand smoke help reduce infection frequency. Improving indoor air quality (ventilation, filtered air) lowers exposure to irritants and may reduce recurrent inflammation.
Importance of Balanced Nutrition and Vitamins
A nutrient-dense diet supports mucosal immunity. Vitamins A, C, D, and zinc have recognized roles in immune function; supplementation should be guided by a clinician when deficiencies are suspected. Balanced nutrition is a long-term preventive strategy rather than a quick fix.
How to Prevent Seasonal Infections
Vaccination, good hand hygiene, and avoiding close contact with sick people during high-transmission seasons reduce the overall burden of infections that can inflame adenoids. Prompt treatment of upper respiratory infections limits the chance of chronic inflammation.
Regular ENT Checkups and Early Detection
For children with recurrent ear infections, breathing problems, or poor sleep, regular ENT follow-up allows proactive management. Early detection and intervention prevent complications like prolonged hearing issues or learning impact.
Lifestyle Adjustments for Better Breathing
Encouraging nasal breathing, maintaining healthy sleep posture, and avoiding mouth breathing when possible supports airway health. Simple breathing exercises and habit coaching can help children transition away from chronic mouth breathing.
12. Living with Adenoidid: Long-Term Care and Support
Managing Chronic Symptoms Safely
Long-term management often blends medical therapy, environmental control, and occasional surgical intervention. Tracking symptom patterns (sleep quality, ear infections, nasal obstruction) helps clinicians tailor care plans. Open communication with an ENT and pediatrician ensures decisions are evidence-based and individualized.
Coping Strategies for Children and Parents
Parents can use structured routines to improve sleep hygiene, create low-allergen sleeping environments, and coordinate school accommodations when necessary. Emotional support, clear explanations, and involving children in simple care tasks reduce anxiety and promote recovery.
Sleep Position and Breathing Exercises
Raising the head of the bed slightly and encouraging side sleeping may reduce nasal obstruction during sleep. Age-appropriate breathing exercises and myofunctional therapy (when recommended by specialists) can support improved nasal breathing over time.
When to Seek Specialist Advice
If conservative measures fail, signs of hearing loss appear, or sleep-disordered breathing persists, consult an otolaryngologist for targeted evaluation. Timely referral avoids prolonged problems and unlocks treatment options that restore healthy breathing and sleep.
Mental and Emotional Health Considerations
Persistent symptoms can affect a child’s social life, school performance, and family stress levels. Addressing emotional impacts and ensuring families have resources and clear plans improves overall outcomes and resilience.
13. Adenoidid vs. Other ENT Conditions
Adenoidid vs. Tonsillitis: Key Differences
Tonsillitis primarily affects the palatine tonsils lower in the throat and often causes sore throat and visible tonsillar swelling. Adenoid problems present with nasal obstruction, snoring, and ear issues. Many children have both adenotonsillar disease simultaneously, which requires a combined clinical approach.
Adenoidid vs. Sinusitis: Overlapping Symptoms
Chronic sinusitis and adenoid hypertrophy share congestion and post-nasal drip. Distinguishing them relies on endoscopy and imaging; sometimes both conditions co-exist and need coordinated treatment.
How Adenoidid Affects Ear Health (Otitis Media Connection)
Enlarged or infected adenoids can block the Eustachian tube opening, leading to otitis media with effusion or recurrent ear infections. Removing adenoids (with or without grommet insertion) is an evidence-supported option in selected children to reduce OME recurrence.
The Role of Allergies and Rhinitis in Adenoid Problems
Allergic rhinitis often coexists with adenoid disease and contributes to persistent inflammation. Treating allergies reduces overall mucosal inflammation and can lower the frequency of adenoid-related symptoms.
15. Expert Advice and Medical Insights
ENT Specialists’ Recommendations
Otolaryngologists recommend individualized care: treat acute infections conservatively, evaluate recurrent or severe symptoms promptly, and consider adenoidectomy when evidence shows benefit (recurrent otitis media, persistent OSA, or obstructive symptoms). Shared decision-making with caregivers yields the best outcomes.
Pediatrician Advice for Parents
Pediatricians focus on symptom tracking, timely antibiotic use only when indicated, and referral to ENT for persistent ear problems, sleep issues, or significant nasal obstruction. Early intervention protects hearing and developmental milestones.
Common Mistakes to Avoid During Treatment
Avoid overuse of antibiotics without clear bacterial evidence, delay ENT referral when warning signs (hearing loss, growth issues, significant sleep apnea) appear, and neglect environmental changes that can reduce recurrence. Evidence-based steps provide safer, more durable results.
Importance of Accurate Diagnosis
Because symptoms overlap with other ENT conditions, accurate ENT examination (including endoscopy and targeted imaging when needed) is crucial to effective and minimally invasive care.
16. When to See a Doctor
Warning Signs That Need Medical Attention
Seek prompt care for high fevers, persistent or worsening ear pain, hearing loss, choking or severe breathing difficulty, daytime sleepiness from poor nighttime breathing, or repeated infections despite treatment. These signs suggest complications that warrant specialist evaluation.
Emergency Symptoms You Shouldn’t Ignore
Stridor (high-pitched noisy breathing), severe respiratory distress, persistent uncontrolled bleeding after an injury, or signs of systemic infection require emergency medical attention. Adenoid problems rarely cause immediate life-threatening events, but airway compromise is urgent when present.
How to Prepare for an ENT Appointment
Bring a symptom diary (sleep, snoring, ear infections), any prior imaging or ENT notes, and a list of medications and allergies. Note behavior changes or school concerns related to sleep or hearing—these details help the specialist assess impact and urgency.
17. Key Takeaways
Summary of Major Causes, Symptoms, and Treatments
Adenoidid, seen as adenoiditis or hypertrophy, often leads to nasal blockage, snoring, ear infections, and sleep troubles in kids.Diagnosis relies on clinical evaluation and endoscopy; treatments range from saline and steroids to antibiotics when indicated, and adenoidectomy for selected, recurrent, or obstructive cases. Evidence supports surgery for recurrent otitis media and sleep-related breathing disorders when medical care fails.
How to Maintain Long-Term Adenoid Health
Control environmental irritants, treat allergies, use supportive nasal care, and pursue prompt medical evaluation for recurrent infections or sleep disturbances. These steps protect hearing, sleep, and quality of life.
Encouraging a Proactive Approach to ENT Wellness
Timely evaluation, evidence-based treatment, and family education create the best outcomes. Knowledge is empowering — recognizing red flags and seeking specialist care when indicated keeps children and adults breathing better and feeling better.
Conclusion
As patient language evolves, terms like adenoidid can help bridge search intent and reliable medical guidance. Quality content that translates medical evidence into clear action improves care-seeking and outcomes for families and adults alike.
This guide is designed to be trusted, actionable, and encouraging: know the signs, try conservative measures safely, and consult an ENT when problems persist. Early action improves sleep, hearing, and overall wellbeing.
Prevention, accurate diagnosis, and targeted treatment are the trio that transforms recurrent adenoid trouble into lasting relief. You don’t have to accept poor sleep or recurring ear infections as “normal” — help is available, and outcomes are excellent with the right approach.
Frequently Asked Questions
Can Adenoidid Go Away Without Surgery?
Yes — many cases, especially viral flares, improve with medical therapy and conservative care. Recurrent problems or structural obstruction may ultimately require surgery.
Is Adenoidid Contagious?
The adenoid inflammation itself is not contagious, but the underlying infections (viral or bacterial) that trigger adenoid swelling can spread between people. Good hygiene limits transmission.
What Age Group Is Most Affected?
Children (especially ages 2–6) are most commonly affected because adenoids are larger and more active in early childhood; adult cases occur but are less frequent.
Can Adenoids Grow Back After Removal?
Regrowth is uncommon but possible, particularly if small residual tissue remains after surgery; most patients see long-term relief following adenoidectomy.
How to Prevent Adenoidid Naturally?
Reduce smoke exposure, maintain good hand hygiene, manage allergies, and use nasal saline to keep mucosa clear. These measures lower infection risk and chronic inflammation.
Stay in touch to get more updates & alerts on Anonib! Thank you